|
| |
 |
Dr S Venkatachalam, MD FRCP
Consultant Rheumatologist
Cannock Chase Hospital, UK |
| Osteoporosis is a systemic skeletal disease characterized by low bone mass and changes in bone microarchitecture leading to increased bone fragility and susceptibility to fractures. Modifications could include the propensity to falls and biochemical turnover of bone. |
|
Dual-energy X-ray absorptiometry (DXA) scan is the best modality for the diagnosis of osteoporosis. |
|
Lack of standardization for the Indian population and comparing against NHANES database may overestimate osteoporosis; falsely elevated spine BMD due to degenerative changes in older patients or fluorosis in endemic areas; cannot be repeated in a short time to assess response to treatment; inaccurate values because of defective mineralization due to osteomalacia. |
|
| Secondary causes of osteoporosis may be present in about 20% of patients and include malabsorption, inflammatory arthritis, diabetes mellitus and chronic liver or renal disease. Full blood count, ESR, glucose, calcium, liver and renal function are essential tests. If necessary, test for 25-hydroxy vitamin D, PTH, serum protein electrophoresis, urine for Bence Jones protein, serum testosterone, LH and FSH can be carried out. |
|
Bone markers are not useful in the diagnosis of osteoporosis, but have a role in monitoring response to therapy in osteoporosis. Serum C-terminal peptide of collagen (CTX), a resorption marker, and serum Procollagen type 1 N terminal propeptide (PINP), a formation marker, are promising. |
|
FRAX is a clinical risk assessment tool adapted in India. It is useful to direct treatment to those patients who have a high risk of an osteoporotic fracture in the next 10 years even without BMD. It has some caveats and needs modifications for steroid dose and vertebral osteoporosis. Intervention thresholds for a major osteoporotic fracture (vary from 2.8% at 50 years to 17% at 75 years or more) or hip fractures have been defined for the Indian setting (see Figs1 and 2).
Fig. 1: Assessment guidelines based on the 10-year probability of a major fracture (%).
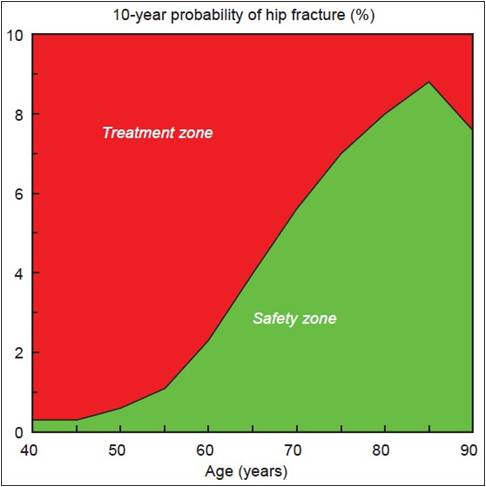 Fig. 2: Assessment guidelines based on the 10-year probability of a hip fracture (%). The sigmoid curve denotes the ‘fracture threshold’ in postmenopausal women from India, which in turn may be considered as an intervention threshold.
Fig. 2: Assessment guidelines based on the 10-year probability of a hip fracture (%). The sigmoid curve denotes the ‘fracture threshold’ in postmenopausal women from India, which in turn may be considered as an intervention threshold.
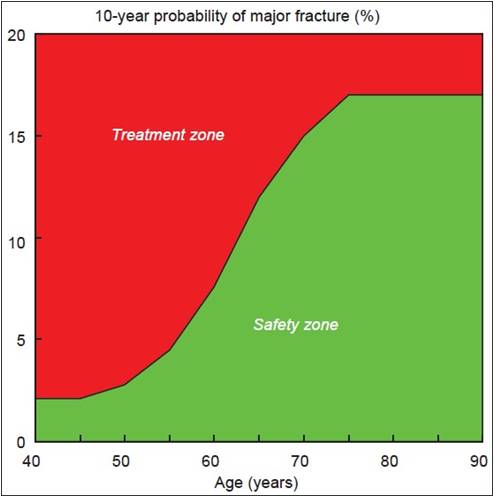
Figures courtesy: Kanis J. Commentary on guidelines on postmenopausal osteoporosis-Indian Menopause Society. J Mid-life Health. 2013;4:129–131.
Available at: http://www.jmidlifehealth.org/text.asp?2013/4/2/129/115297 |
|
Hypogonadism, multiple myeloma, Cushing’s syndrome, organ transplantation. |
|
Oral bisphosphonates–Alendronic acid or Risedronate—are the first-line treatment option for osteoporosis. They need to be given with adequate calcium and vitamin D supplements. If someone is unable to take an oral bisphosphonate or intolerant, I.V. bisphosphonate is preferred. Teriparatide is reserved for those with severe osteoporosis and multiple fractures. |
|
| Vertebroplasty or kyphoplasty can be useful in a selected group of patients with severe ongoing spinal pain after failure of optimal pain management for at least 3 weeks after a vertebral fracture. They are very expensive and need to be undertaken in specialist centers only if the location of pain correlates with the site of fracture on imaging and if bone edema is present in the MRI. They are associated with complications like cement leakage and neurological problems and fractures above and below. The patients also need treatment for osteoporosis. |
|
At least 2 weeks after a fracture. |
|
Calcium 1000 mg and vitamin D 800 U/day need to be supplemented in the management of patients with osteoporosis after correction of vitamin D deficiency when necessary with high-dose vitamin D up to 300,000 U. |
|
Most of the studies show no increase in stone risk with high calcium intake (from either diet or supplements). Contrariwise, there is a substantial body of evidence, both from controlled trials and from observational studies, indicating that there is an inverse relationship between calcium intake and stone risk.
However, in an individual with known stone disease, it may be worthwhile to do 24-hour urinary calcium excretion test and then decide regarding the quantum of calcium therapy.
- Hearney RP. Calcium supplementation and incident kidney stone risk: A systematic review. J Am Coll Nutr. 2008;27(5):519–527.
- Grases F, Costa-Bauza A, Prieto RM. Renal lithiasis and nutrition. Nutr J. 2006;5:23.
|
|
Choice of Medication for Osteoporosis:
First-line: Oral bisphosphonates, Alendronate, Risedronate or Ibandronate (weekly or monthly)—less expensive, effective but inconvenient for some, poor compliance.
Second-line: In patients with swallowing difficulty or esophagitis or intolerance for oral bisphosphonates—I.V. bisphosphonate (Ibandronate) once every 3 months/Zoledronic acid once a year (contraindicated in patients with eGFR <35 mL/min) 100% compliance.
Third-line: Teriparatide—in patients with severe osteoporosis and multiple vertebral fractures, it is given for up to 18-24 months followed by a bisphosphonate.
Others: Strontium ranelate may be suitable for a selected group of elderly patients who cannot have bisphosphonates but without cardiovascular risk factors.
Raloxifene may be an option for younger women with vertebral osteoporosis alone and risk of breast cancer.
Hormone replacement therapy for a few years may be an option for younger women with premature menopause or within the first 5–10 years after menopause if they have menopausal symptoms and not suitable for other therapies. |
|
Teriparatide is most suitable for those with severe osteoporosis and multiple fractures, as it is anabolic. However, it is expensive, and should be avoided in case of hyperparathyroidism, severe renal failure, Paget’s disease of the bone or bone metastases. |
|
Newer Medications
Denosumab: This is a monoclonal antibody against RANK ligand, antiresorptive, very convenient and effective, given as 6-monthly subcutaneous injections, well-tolerated, can be used in moderate renal failure.
Romosozumab: This is a monoclonal antibody that binds to sclerostin, anabolic, given as monthly injection.
Odanacatib: This is a cathepsin K inhibitor, indicated as weekly oral preparation, antiresorptive, effective in men and women.
Therapeutic strategies: Combination of teriparatide and I.V. zoledronate is indicated in severe osteoporosis. Review long-term bisphosphonate therapy (after 5 years for oral and after 3 years for I.V.) and continue treatment if fracture risk continues to be high. |
|
|
|
 |
|